Items filtered by date: Friday, 25 April 2025
Demystifying Morton's Neuroma
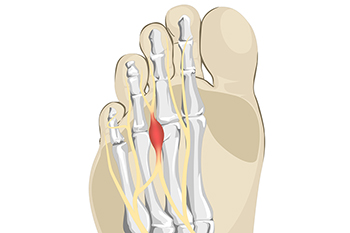
Morton's neuroma, named after the American surgeon Thomas G. Morton who first described it in the 19th century, is a painful condition affecting the nerves in the foot. This benign growth typically forms between the third and fourth toes, resulting from compression or irritation of the interdigital nerve. The exact cause of Morton's neuroma remains elusive, but factors such as wearing tight or high-heeled shoes, engaging in repetitive high-impact activities, or foot deformities may contribute to its development. Symptoms of Morton's neuroma often include a sharp, burning pain or sensation of a lump or foreign object in the ball of the foot. Individuals may also experience numbness, tingling, or a feeling of walking on a pebble. As the condition progresses, discomfort may worsen and become more persistent, particularly during weight-bearing activities. If you have pain in this part of your foot, it may be Morton's neuroma, and it is suggested that you visit a podiatrist. This type of doctor can accurately diagnose and effectively treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Patrick Bruton, DPM of Big Country foot and Ankle. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Symptoms and Diagnosis of Athlete's Foot

Athlete's foot is a common fungal infection affecting the skin on the feet, particularly between the toes. Symptoms include itching, burning, and stinging sensations, often accompanied by redness, peeling, and cracking skin. The affected areas may also appear swollen and develop blisters. Diagnosis typically involves a physical examination by a podiatrist, who may scrape a small sample of the affected skin to examine under a microscope or send it to a lab for testing. Identifying the presence of fungal elements confirms the diagnosis. Early recognition and treatment of athlete's foot are essential to relieve discomfort and prevent the infection from spreading. Proper hygiene, antifungal medications, and keeping the feet dry and clean are effective measures to manage and prevent athlete's foot. Athlete’s foot can be uncomfortable and unsightly. If you have any of the above symptoms, it is suggested that you consult a podiatrist who can successfully treat this condition, which may include prescribed medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Arthritis Can Cause Pain in the Feet and Ankles
Diabetic Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If bone is removed it is then replaced with prostheses, or synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
What Does Diabetic Limb Salvage Mean?

Diabetic limb salvage is a medical approach focused on preventing amputations in patients with diabetes. Diabetes can lead to poor circulation and nerve damage, particularly in the lower extremities, increasing the risk of severe infections and ulcers. Limb salvage involves a comprehensive treatment plan aimed at healing these ulcers, improving blood flow, and managing infections. This multidisciplinary approach includes wound care, surgical interventions, and lifestyle modifications to control blood sugar levels and enhance overall foot health. The goal is to preserve the patient's limbs, improve quality of life, and prevent the devastating impact of amputation. Timely intervention and continuous care are essential to the success of diabetic limb salvage, emphasizing the importance of regular medical check-ups and early treatment of any foot issues in diabetic patients. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can evaluate your condition, and educate you about methods that may help to avoid amputation.
Diabetic Limb Salvage
Diabetic limb salvage can be an effective way in preventing the need for limb amputation. If you have a foot ulcer and diabetes, consult with Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Diabetic Limb Salvage?
Diabetic limb salvage is the attempt of saving a limb, such as the foot, that has an infected ulcer, from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
Diabetes is the number one cause of non-traumatic amputations in the United States. Amputation has been found to lead to higher mortality rates. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Treatment of Adult Acquired Flat Feet

Adult-acquired flatfoot, also known as posterior tibial tendon dysfunction, can be a source of significant discomfort for many adults. Adult-acquired flatfoot develops when the posterior tibial tendon weakens, causing the arch of the foot to collapse gradually. Symptoms can include pain along the inside of the ankle, swelling, difficulty standing on tiptoes, and increased discomfort during weight-bearing activities. A podiatrist can perform an assessment of your foot's flexibility and alignment, and may order X-rays or other imaging techniques to assess the condition of the tendon and bones. Treatment options typically start conservatively with custom orthotics or ankle braces to support the foot and alleviate pain. Activity modifications and anti-inflammatory medications may also be recommended. In cases where conservative treatments do not provide sufficient relief, surgical tendon repair or fusion procedures may be considered to restore stability and function to the affected foot. If you are experiencing problems related to flat feet, it is suggested that you schedule an appointment with a podiatrist for treatment.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.
Treatment for Broken Ankles
 Broken ankles, or ankle fractures, occur when one or more bones in the ankle joint break due to trauma. This injury can result from falls, sports activities, car accidents, or any situation where the ankle twists or experiences a heavy impact. Symptoms can include severe pain, swelling, bruising, and an inability to bear weight on the affected foot. Treatment depends on the severity of the fracture. Minor fractures may only require immobilization with a cast or brace to allow the bones to heal naturally. More severe fractures, where bones are displaced, might need surgical intervention to realign and stabilize the bones with pins, plates, or screws. Rehabilitation focuses on restoring strength, flexibility, and function through exercises. These exercises might include range-of-motion activities, balance training, and gradual weight-bearing exercises. Prompt and effective treatment is important for optimal recovery. If you suspect a broken ankle, it is suggested that you visit a podiatrist for a proper diagnosis and a tailored treatment plan.
Broken ankles, or ankle fractures, occur when one or more bones in the ankle joint break due to trauma. This injury can result from falls, sports activities, car accidents, or any situation where the ankle twists or experiences a heavy impact. Symptoms can include severe pain, swelling, bruising, and an inability to bear weight on the affected foot. Treatment depends on the severity of the fracture. Minor fractures may only require immobilization with a cast or brace to allow the bones to heal naturally. More severe fractures, where bones are displaced, might need surgical intervention to realign and stabilize the bones with pins, plates, or screws. Rehabilitation focuses on restoring strength, flexibility, and function through exercises. These exercises might include range-of-motion activities, balance training, and gradual weight-bearing exercises. Prompt and effective treatment is important for optimal recovery. If you suspect a broken ankle, it is suggested that you visit a podiatrist for a proper diagnosis and a tailored treatment plan.
Broken ankles need immediate treatment. If you are seeking treatment, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.

