Treatment of Adult Acquired Flat Feet

Adult-acquired flatfoot, also known as posterior tibial tendon dysfunction, can be a source of significant discomfort for many adults. Adult-acquired flatfoot develops when the posterior tibial tendon weakens, causing the arch of the foot to collapse gradually. Symptoms can include pain along the inside of the ankle, swelling, difficulty standing on tiptoes, and increased discomfort during weight-bearing activities. A podiatrist can perform an assessment of your foot's flexibility and alignment, and may order X-rays or other imaging techniques to assess the condition of the tendon and bones. Treatment options typically start conservatively with custom orthotics or ankle braces to support the foot and alleviate pain. Activity modifications and anti-inflammatory medications may also be recommended. In cases where conservative treatments do not provide sufficient relief, surgical tendon repair or fusion procedures may be considered to restore stability and function to the affected foot. If you are experiencing problems related to flat feet, it is suggested that you schedule an appointment with a podiatrist for treatment.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Treatment for Broken Ankles
 Broken ankles, or ankle fractures, occur when one or more bones in the ankle joint break due to trauma. This injury can result from falls, sports activities, car accidents, or any situation where the ankle twists or experiences a heavy impact. Symptoms can include severe pain, swelling, bruising, and an inability to bear weight on the affected foot. Treatment depends on the severity of the fracture. Minor fractures may only require immobilization with a cast or brace to allow the bones to heal naturally. More severe fractures, where bones are displaced, might need surgical intervention to realign and stabilize the bones with pins, plates, or screws. Rehabilitation focuses on restoring strength, flexibility, and function through exercises. These exercises might include range-of-motion activities, balance training, and gradual weight-bearing exercises. Prompt and effective treatment is important for optimal recovery. If you suspect a broken ankle, it is suggested that you visit a podiatrist for a proper diagnosis and a tailored treatment plan.
Broken ankles, or ankle fractures, occur when one or more bones in the ankle joint break due to trauma. This injury can result from falls, sports activities, car accidents, or any situation where the ankle twists or experiences a heavy impact. Symptoms can include severe pain, swelling, bruising, and an inability to bear weight on the affected foot. Treatment depends on the severity of the fracture. Minor fractures may only require immobilization with a cast or brace to allow the bones to heal naturally. More severe fractures, where bones are displaced, might need surgical intervention to realign and stabilize the bones with pins, plates, or screws. Rehabilitation focuses on restoring strength, flexibility, and function through exercises. These exercises might include range-of-motion activities, balance training, and gradual weight-bearing exercises. Prompt and effective treatment is important for optimal recovery. If you suspect a broken ankle, it is suggested that you visit a podiatrist for a proper diagnosis and a tailored treatment plan.
Broken ankles need immediate treatment. If you are seeking treatment, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.
How Flip-Flops Affect the Feet

Flip-flops are a popular choice for summer footwear, but they can significantly impact foot biomechanics compared to walking barefoot. Studies comparing traditional flip-flops with more structured versions have highlighted differences in ankle movement and ground reaction forces. Traditional flip-flops often increase dorsiflexion, or the upward bending of the foot at the ankle as you walk. This happens because the toes grip to keep the shoe on. More structured flip-flops reduce ankle eversion, which is the outward rolling of the foot when you stand. This design offers better support and may lower the risk of overuse injuries by minimizing excessive ankle movement and reducing impact at the heel when your foot lands. Even so, the inherent design of flip-flops, which often requires gripping with the toes, can lead to discomfort and long-term foot issues. This gripping action can strain the muscles and tendons, leading to plantar fasciitis or tendonitis, among other problems. While flip-flops provide short-term convenience, they may not be ideal for prolonged use or activities that require a lot of walking. To ensure your footwear supports your foot health effectively or to address foot pain, it is suggested that you schedule an appointment with a podiatrist.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flip Flops and Feet
Flip flops are often a popular choice of footwear for many people. Flip flops allow your feet to breathe and give your toes the freedom of movement. They are easy to slip on and can be worn with virtually any style of clothing. Flip flops, however, despite their many benefits, can be detrimental for your foot health.
Despite their comfortableness, frequently wearing flip flops can create problems in the lower body over time. Issues mainly stem from the fact that people walk differently in flip flops compared to other footwear, such as sneakers. This is due to a change in one’s natural gait, which therefore creates stress in different parts of the body while hindering the body’s natural posture. Problems can also arise in the arches and balls of the feet. Flip flops provide little to no support to these areas.
Aside from long-term problems, flip-fops can also create short-term issues as well, such as ankle sprains and blisters. Weak materials that are flexible and bendable are generally used to manufacture flip flops. These materials make its wearers prone to both tripping and injuring their ankles. Flip flops can create blisters as the material rubs against the foot. People are much more at risk for infection while wearing flip flops due to their openness. This also makes it easier to scrape and cut the foot since there is a lack of protection. If these cuts are left untreated and uncovered, the risk then becomes greater.
To prevent the aforementioned occurrences, purchase a pair of flip flops that offer significant protection. The soles of the flip flops should not be floppy, but sturdy and firm, and should not significantly bend or wiggle when lifted from the floor. Flip flops made of high-quality materials will not be affected by this problem. While higher quality flip flops may be more expensive, they will last longer and provide better protection compared to a cheaper pair. Brand name flip flops sold from a quality manufacturer are a dependable option.
There is no problem in wearing your favorite pair of flip flops so as long as you do not wear them daily or for extended periods of time. Flip flops should be replaced every 3-4 months to ensure that they provide your feet with the best protection.
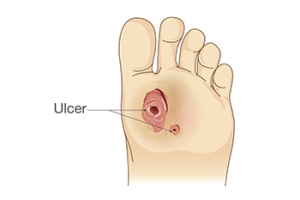
How Podiatrists Can Help With Diabetic Foot Ulcers
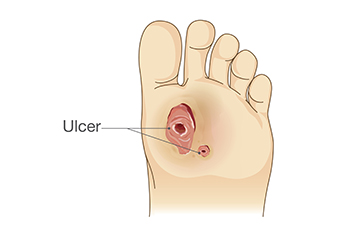 Diabetic foot ulcers are open sores or wounds that develop on the feet of individuals with diabetes. Ulcers may arise due to poor blood circulation, nerve damage known as neuropathy, and high blood sugar levels, which impair the body's ability to heal. Symptoms include redness, swelling, and drainage from the ulcer, and they may become infected if not properly treated. Some risk factors for diabetic foot ulcers are prolonged diabetes, poor glycemic control, smoking, and wearing inappropriate footwear. Additionally, foot deformities and a history of foot ulcers or amputation increase the likelihood of developing these sores. Treatment involves keeping the ulcer clean and covered, managing blood glucose levels, and taking antibiotics to prevent or treat infection. A podiatrist plays a crucial role in managing and preventing diabetic foot ulcers. They can provide routine foot care, recommend proper footwear, and offer guidance on foot hygiene. If you have diabetes and notice any foot abnormalities, it is strongly suggested that you schedule an appointment with a podiatrist to prevent complications.
Diabetic foot ulcers are open sores or wounds that develop on the feet of individuals with diabetes. Ulcers may arise due to poor blood circulation, nerve damage known as neuropathy, and high blood sugar levels, which impair the body's ability to heal. Symptoms include redness, swelling, and drainage from the ulcer, and they may become infected if not properly treated. Some risk factors for diabetic foot ulcers are prolonged diabetes, poor glycemic control, smoking, and wearing inappropriate footwear. Additionally, foot deformities and a history of foot ulcers or amputation increase the likelihood of developing these sores. Treatment involves keeping the ulcer clean and covered, managing blood glucose levels, and taking antibiotics to prevent or treat infection. A podiatrist plays a crucial role in managing and preventing diabetic foot ulcers. They can provide routine foot care, recommend proper footwear, and offer guidance on foot hygiene. If you have diabetes and notice any foot abnormalities, it is strongly suggested that you schedule an appointment with a podiatrist to prevent complications.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Causes And Treatment Of Cracked Heels

Cracked heels often stem from various factors, including obesity, wearing ill-fitting shoes, prolonged standing, and dry skin. When the skin on your feet lacks moisture and becomes stiff, it is more susceptible to cracking, especially under pressure while standing or walking. Certain conditions, such as diabetes, psoriasis, and flat feet, can further dry out the skin and increase the risk of cracked heels or painful fissures. Preventative measures include moisturizing regularly, avoiding harsh soaps, and opting for closed-heeled shoes with ample cushioning. Wearing cotton socks can also help to reduce friction. Mild relief typically involves moisturizers containing ingredients like urea or hyaluronic acid, which help retain moisture and soften the skin. While mild cases can often be managed at home, it is important to see a podiatrist if heel cracks are associated with a medical condition or if they have become infected. Seeking professional advice ensures a proper diagnosis and treatment, leading to quicker healing and long-term foot health. If cracked and painful heels are causing you discomfort, it is suggested that you schedule an appointment with a podiatrist.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.